Illustration by Marta Pucci
What are the best non-hormonal birth control options?
Exploring 12 non-hormonal methods

Top things to know:
Some non-hormonal birth control methods need your attention with each use, while others last for years or are permanent
While hormonal birth control is safe for most people, it may not be a good option if you have heart disease, recently gave birth, or don’t like the side effects
Condoms are an affordable and accessible type of non-hormonal birth control that protect against both pregnancy and sexually transmitted infections (STIs)
Fertility awareness-based methods (FABMs) may be a good option if you want to avoid hormonal birth control and learn more about your body
All you need to know about non-hormonal birth control
If you visit a healthcare provider to talk about birth control, hormonal methods are often presented as the best option. That’s because hormonal birth control generally has higher rates of efficacy, meaning it’s more likely to prevent pregnancy if used as directed (1). However, everyone is unique, and so are their birth control needs—so hormonal birth control might not be the right choice for everyone (2).
Non-hormonal birth control doesn’t contain hormones (1). Each type works differently, but none of them rely on hormones to prevent pregnancy (1). If hormonal birth control isn't suitable for you or you're interested in non-hormonal options, we’ve listed the 12 types in this article.

Why choose non-hormonal birth control?
People often choose non-hormonal birth control because they don’t like the side effects of hormonal methods (3). Some have medical reasons for avoiding hormonal birth control—for example, those who experience migraines or heart disease might choose to avoid it (1,4). This is because the hormones in birth control can cause changes in blood clotting, putting these individuals at a higher risk of developing blood clots (1). Other people may have personal reasons for wanting to avoid hormonal birth control.
How effective is non-hormonal birth control compared to hormonal?
Non-hormonal birth control can be effective if used correctly every time. It’s hard to compare its effectiveness to hormonal birth control because this depends on proper use. Each non-hormonal birth control has pros and cons, including different rates of efficacy. When choosing a method, consider your main goal (such as preventing pregnancy) and how comfortable you are with the possibility of becoming pregnant if the method fails.
Types of non-hormonal birth control
When choosing a form of non-hormonal birth control, consider how it’s used, its typical effectiveness, and how well it suits your needs.
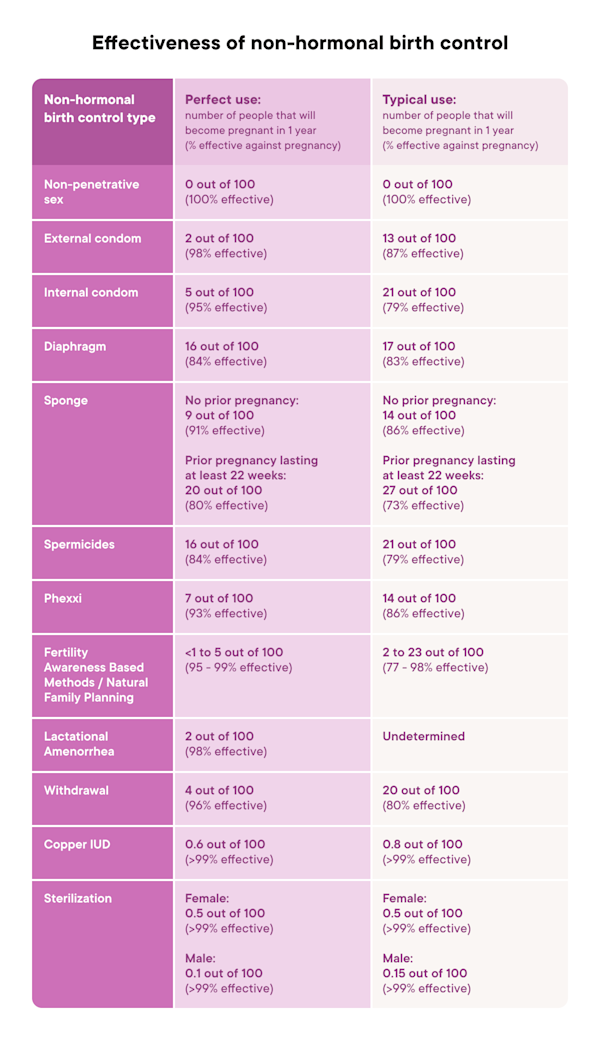
The effectiveness of birth control is described in two ways:
Typical use: Describes using a method like an average person does (1). This includes inconsistent or incorrect use (1).
Perfect use: Describes using a method exactly as directed every single time (1).
Among Clue users who track a non-hormonal method of birth control, the most commonly used methods are:
Condoms: 22% (of these users)
Copper IUD: 15% (of these users)
Fertility Awareness-Based Methods (FABMs): 4% (of these users)
What are my non-hormonal birth control options?
If hormonal contraception isn’t for you, there are many valid non-hormonal options (1). These include permanent sterilization, copper intrauterine devices (IUDs), barrier methods (like spermicides and condoms), as well as the withdrawal method, and fertility awareness-based methods (FABMs) (1).
Here’s our full list of non-hormonal birth control options:
1. Non-penetrative sex
Non-penetrative sex (noncoital sex or outercourse) is sexual activity that does not involve inserting anything into the vagina, anus, or mouth (1). This can include kissing, hugging, handjobs, dry humping, masturbating with a partner, using vibrators or toys, watching porn with a partner, massage, and breast play. For some people, these activities can provide just as much sexual pleasure as intercourse.
Unintended pregnancy within one year of using only non-penetrative sex as birth control:
Typical use: In moments of intimacy, non-penetrative sex can “accidentally” lead to penetrative sex. Pregnancy or STIs can occur if another form of birth control is not used (1).
Perfect use: Non-penetrative sex prevents pregnancy and STIs if bodily fluids from one person do not touch the other (1).
2. External “male” condoms
External ("male") condoms are barrier methods that protect against pregnancy and STIs if used as directed every single time (1). They are easy to find, affordable, and sometimes even free, making them the preferred birth control option for many people. Condoms come in many styles, shapes, colors, and flavors (1). Adding lubrication (lube) can help make sex with a condom more enjoyable (5).
Types of external condoms:
Latex: This is the most common type. Only water- or silicone-based lubricants can be used with these (1).
Plastic (Polyurethane): These may be useful for those with latex allergies. They can be used with oil-based lubes (1).
Natural membrane (“Lambskin”): These may also be useful for those with latex allergies. They do not protect against STIs due to having tiny pores that could allow viruses to pass through (6). Any type of lubrication can be used with these (7).
Unintended pregnancy rates within one year of using only external condoms for birth control (1):
Typical use: 13% (13 out of 100)
Perfect use: 2% (2 out of 100)
3. Internal “female” condoms
The internal (“female”) condom is a barrier method that is typically less effective than the external (“male”) condom. Female condoms are made of special plastics (polyurethane or nitrile) and are placed inside the vagina or anus during intercourse (1). The internal condom has a ring on either end—one to hold it in place and the other to prevent it from sliding too far into the vagina (which could increase the chance of pregnancy) (1). Female condoms can be inserted up to eight hours before having sex (6).
Unintended pregnancy rates within one year of using only internal condoms for birth control (1):
Typical use: 21% (21 out of 100)
Perfect use: 5% (5 out of 100)
4. Diaphragm and cervical cap
Diaphragms and cervical caps are barrier methods made of silicone. They are placed over the cervix (the opening of the uterus from the vagina) and used with spermicide (1). Cervical caps are smaller and fit tightly around the cervix (1), while diaphragms stay in place by sitting behind the pubic bone (1). Neither method protects against STIs (1).
Diaphragms and cervical caps are available in the USA with a prescription. An OB/GYN, women’s health nurse practitioner, doctor, or midwife fits the diaphragm or cervical cap the first time to pick the right size. The healthcare provider inserts the index and middle finger into the vagina to feel where the device sits (1). There’s also a one-size-fits-all diaphragm, called Caya, available (8). A healthcare provider may have you insert Caya during the visit and then perform a pelvic exam to check it was placed in the right position (8). Water-based spermicide should also be used with Caya (8).
Only use water-based spermicides or lubricants when using a diaphragm and a cervical cap, as oil-based products can cause a cervical cap or diaphragm to break down (1).
Unintended pregnancy within one year of using cervical barrier methods for birth control (1):
Typical use: 17% (17 out of 100)
Perfect use: 16% (16 out of 100)
5. Contraceptive sponge
The contraceptive sponge is a barrier method filled with spermicide that’s placed in the vagina before sex. It must be left in for six hours after sexual activity to be effective (1). The sponge is available over the counter, but it’s not as effective as the diaphragm (1). It can be used along with condoms.
Unintended pregnancy rates within one year of using the contraceptive sponge for birth control:
In people who have never been pregnant (1):
Typical use: 14% (14 out of 100)
Perfect use: 9% (9 out of 100)
In people who have had a prior pregnancy lasting 22 weeks or longer (1):
Typical use: 27% (27 out of 100)
Perfect use: 20% (20 out of 100)
6. Spermicides
Spermicides are barrier methods that are often used with condoms, cervical caps, and/or diaphragms to make them more effective (1). They are available as small solid capsules (suppositories), foams, vaginal gels, and creams (1). Spermicides slow down or destroy sperm and stop them from entering the cervix (1). Frequent use of spermicides may make some people more susceptible to HIV, so it’s only recommended if both partners’ risk of HIV is low (1).
Apply spermicide close to the cervix. Do this by inserting the applicator, suppository, or cream into the vagina as far as you can (1).
Unintended pregnancy rates within one year of using only spermicides for birth control (1):
Typical use: 21% (21 out of 100)
Perfect use: 16% (16 out of 100)
7. Phexxi (EVO100)
Phexxi is a non-hormonal vaginal gel barrier method that can be used without a condom (1,9). It is not a spermicide; it works by lowering the vagina’s pH, making it more acidic (9). This makes it difficult for sperm to move (9).
Insert Phexxi into the vagina immediately before, or up to one hour before, sex using the applicator (9).
In a study, some people who used Phexxi experienced vaginal burning and itching, yeast infections, or urinary tract infections (UTIs), but most people didn’t (9). Since the chance of UTIs might increase on Phexxi, talk to your healthcare provider before using Phexxi if you’ve had multiple UTIs or other urinary tract conditions (10). In the trial study of Phexxi, fewer than 1% of people experienced any urinary tract infections, and only one person had a serious infection (10).
Unintended pregnancy rates within one year of using Phexxi for birth control (1):
Typical use: 14% (14 out of 100)
Perfect use: 7% (7 out of 100)
8. Breastfeeding/chest feeding (lactational amenorrhea or LAM)
Lactational amenorrhea (LAM) relies on breastfeeding/chest feeding to prevent ovulation (1). When a baby sucks on the breast/chest, the hormones that usually cause the menstrual cycle are suppressed (1). Without the right amount of these hormones, ovulation won’t happen (1).
Three things must be present for LAM to be effective (11):
You’ve had no menstrual bleeding since giving birth
You are six months or fewer postpartum
You breastfeed/chest feed every 4 hours throughout the day and every 6 hours at night, and use no more than 15% formula or pumped milk
Unintended pregnancy rates within one year of using breastfeeding for birth control (1):
Typical use: There isn’t an exact rate for lactational amenorrhea (LAM). One study from the 1990s looked at women who returned to work postpartum and were not able to breastfeed their infants on demand. It found the rate of unintended pregnancy increased to around 5% (12).
Perfect use: 1-2% (1-2 out of 100)
9. Withdrawal (the pull-out method)
The withdrawal method involves removing the penis from the vagina before ejaculation (1). It does not protect against STIs. Couples who use withdrawal correctly each time may find it works well for them (1). Perfect use can be difficult and the chance of pregnancy increases with typical use (1).
A few small studies have found that pre-ejaculatory fluid (precum) may contain sperm (13). This means that even if a person removes their penis (pulled out) before they orgasm, some sperm could enter the body through the vagina and result in a pregnancy (18).
Unintended pregnancy rates within one year of using withdrawal for birth control (1):
Typical use: 20% (20 out of 100)
Perfect use: 4% (4 out of 100)
10. Copper IUD
The copper intrauterine device (IUD) is a hormone-free method that lasts for ten years and can also be used as emergency contraception (1). It's easy to take out, and you can also become pregnant right after removal (14).
The copper IUD is a T-shaped piece of plastic wrapped in a thin copper wire that sends out copper ions, making it difficult for sperm to move and reach an egg (15).
Some people can experience heavier bleeding, increased period pain, and cramping while using the copper IUD, but this is likely to get better with time (15). Up to 12 out of 100 people with a copper IUD have the device taken out before the end of the first year because of these side effects (15).
Unintended pregnancy rates within one year of using the copper IUD for birth control (1):
Perfect use (All use is considered perfect use since the copper IUD doesn’t need any maintenance after it’s inserted): Less than 1% (<1 out of 100)
11. Sterilization (tubes tied or vasectomy)
The most popular method of contraception in the USA and around the world is tubal ligation/removal, which is a sterilization procedure for people with uteruses (1). This is a surgical procedure that involves cutting/tying the fallopian tubes or removing the fallopian tubes entirely (1).
Vasectomy is the sterilization procedure for people with scrotums/testes (1). It involves clipping, cutting, or sealing off the vas deferens tube, which transports sperm from the testes to the urethra before ejaculation (1).
Sterilization is a permanent birth control option. Reversals (undoing a procedure) are possible, however they do not always work (1). There is a 4–8% chance of ectopic pregnancy after tubal ligation reversal (1). Instead of a reversal, in vitro fertilization (IVF) is an alternative option for trying to conceive after having a tubal ligation.
Vasectomies require follow-up appointments to ensure that sperm is no longer present in the ejaculate. Backup contraception is needed for the first few months after the procedure has taken place (1).
Unintended pregnancy rates within one year of using sterilization for birth control (1):
Perfect use (All use is considered perfect use, as sterilization doesn’t require any maintenance, except for the initial follow-up appointment after a vasectomy): Less than 1% (<1 out of 100)
12. Fertility awareness-based methods (FABMs)
Fertility awareness-based methods (FABMs), also called natural family planning, follow the changes in the menstrual cycle to predict ovulation and identify the days when sex could lead to pregnancy (1). To prevent pregnancy during those days, people can avoid sex or use a barrier method like a condom (12). To understand how FABMs work, it’s important to understand the basics of the menstrual cycle.
FABMs don’t involve hormones and are often free or cheaper than other birth control methods (1). FABMs don’t protect against STIs.
Unintended pregnancy rates within one year of using FABMs:
Typical use: Ranges from 2-23% (2 to 23 out of 100) depending on the method (1).
Perfect use: Ranges from less than 1-5% (<1 to 5 out of 100) depending on the method (1).
Types of FABMs
There are a few types of FABMs, each with its own “rules”. Some are more effective than others, but none are effective if you do not use them as directed. They include the following methods:
Rhythm (Calendar) method
Standard Days method
TwoDay method
Billings Ovulation method
Sensiplan/Symptothermal method
Not all FABMs are equally effective
Methods like the Rhythm (Calendar) method or Standard Days method assume that the menstrual period always follows a certain number of days and that ovulation happens on the same day each cycle (17). A person trying to avoid pregnancy is instructed to avoid sex or use another birth control method on the days around their ovulation (17). Sometimes people monitor their body temperature. These methods work best for people with predictable cycles that last 26–32 days (17).
Note: The predicted fertile window and ovulation date shown in the Clue app are only estimates and should not be relied upon as a method of contraception.
Cycles are as unique as the people who have them, and not all people with periods have 28-day cycles (1). That means that ovulation may not happen on day 14 each month (1). Predicting ovulation can be tricky in these cases. Getting experience through practice or training may help (17). There might be instructors or support groups in your area or online that can help.
Should I use a fertility awareness-based method?
You may want to consider other types of birth control that don’t require ovulation predictions if any of the following applies to you (17):
Becoming pregnant would be dangerous to your health or damaging to your life
You recently started having periods
You are approaching menopause
You just stopped hormonal birth control
You recently gave birth
Your periods are unpredictable
You have a high risk of getting an STI
You are not able to avoid sex or use a barrier method during days with a high risk of becoming pregnant
Your partner is not willing to participate in using the method correctly
Download Clue to track your birth control method
Choosing to start or stop any form of birth control may come with changes in your body throughout your cycle. You might want to track your mood, skin, sex life, PMS symptoms, or any other changes because these things might fluctuate depending on where you are in your cycle.
Once you download and start using the Clue app, you can enter the type of birth control you’re using—whether it’s hormonal or non-hormonal. If you stop using your form of birth control at any point, continuing to track your symptoms can help give you deeper insight into how your body responds.
FAQs
What is the best non-hormonal birth control?
The method that will work best for you is the one you will use correctly and consistently (1). A birth control method might have a high efficacy rate on paper, but if you are not able to use it the way it is designed, it won’t be effective. This is especially true for non-hormonal birth control. If you don’t keep condoms on hand, prefer not to pause to use them, or your partner isn’t on board with them, they probably aren’t the right choice for you (17).
Is there a birth control pill that doesn't have hormones?
All birth control pills contain hormones and many contain low doses (1). Talk to your healthcare provider to find a birth control pill that works for you. If hormones aren’t an option, you may want to consider a non-hormonal birth control method.
What are the negative side effects of non-hormonal birth control?
Side effects of non-hormonal birth control vary from person to person. Check the packaging of your chosen method for details, but keep in mind that not everyone will experience the full list of symptoms. Most non-hormonal methods (except the copper IUD) are managed by you, so they can be stopped at any time if negative side effects occur.